Role of Pharmacy Benefit Managers in the Pharmaceutical Supply Chain
Pharmacy benefit managers play a central role in determining the cost of medications to consumers.

Source: Getty Images
- As the healthcare industry works to tackle skyrocketing spending, a keen eye is turning toward the pharmaceutical industry. And with that, experts are examining the role pharmacy benefits managers play in the pharmaceutical supply chain and how they impact prescription drug costs.
A pharmacy benefits manager (PBM) is a middleman of sorts that handles most aspects of the drug purchasing process on behalf of private payers, federal and state programs, large employers, and other payer types, according to the Commonwealth Fund.
“By negotiating with drug manufacturers and pharmacies to control drug spending, PBMs have a significant behind-the-scenes impact in determining total drug costs for insurers, shaping patients' access to medications, and determining how much pharmacies are paid," Commonwealth Fund has noted. "PBMs have faced growing scrutiny about their role in rising prescription drug costs and spending."
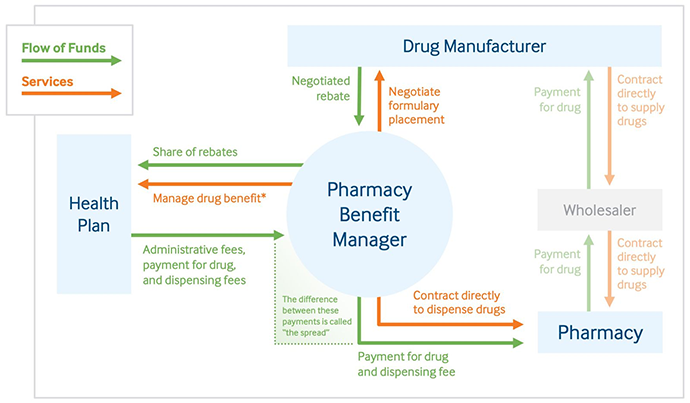
Specifically, PBMs maintain relationships with three key stakeholders in the pharmaceutical supply chain:
- PBM and drug manufacturer: The PBM negotiates a drug price and rebates from the manufacturer. In exchange for rebates, PBMs will put certain drugs on formularies, which ensures a drug manufacturer will get business.
- PBM and health payer: The PBM manages a payer's drug formulary list (i.e., the medications for which plan beneficiaries may receive coverage.) In exchange, the payer gives the PBM money for administrative services, paying for the actual drug, and paying for drug dispensing. Drug rebates the PBM obtained from the manufacturer should factor into the lump sum the payer owes.
- PBM and the pharmacy: In some cases, a PBM will contract with a pharmacy to dispense drugs directly. They will also pay the pharmacy a drug dispensing fee.
Source: The Commonwealth Fund
PBMs are a vital part of the pharmaceutical supply chain that few consumers even know exist, let alone understand. However, their roles ultimately boil down to two principal functions: managing health payer drug formularies and negotiating drug prices and rebates with prescription drug manufacturers.
Maintain drug formulary lists
Central to the job of a PBM is managing and maintaining a healthcare payer’s formulary list.
A drug formulary is a list of prescription drugs that are preferred under a specific health plan. Also referred to as a drug list, formularies are essential to understanding healthcare benefits and what type of care a beneficiary can access.
If a patient is prescribed a drug that is not a part of her health plan's formulary list, either she will pay the entire cost out-of-pocket or her provider will have to select another drug that is under the plan's formulary.
Part of setting that drug formulary is determining patient access to a drug and a drug’s utilization, Commonwealth Fund says. Specifically, PBMs may create medication adherence programs and set up utilization management systems, such as prior authorization or step therapy.
If a drug requires prior authorization, a patient and her provider must obtain specific direction from a board of providers and other stakeholders from the payer for the patient to access the drug. Step therapy requires patients to use lower-cost treatments first, ruling out care options until they move further up the drug formulary.
A PBM's key role in setting a payer's formulary has opened the door to its next job function: negotiating drug costs and, in many cases, managing rebates from prescription drug manufacturers.
Negotiating drug prices, managing rebates
The next leg of a PBM's job is to negotiate a purchasing price from a prescription drug manufacturer. Drug manufacturers are in charge of setting a raw price, known as the list price, for its medications. The list price may be the baseline value manufacturers say their drugs hold, but it is rarely the price a PBM pays for the drug.
Drug manufacturers know that PBMs are responsible for creating drug formularies. And because the manufacturer wants its drugs – especially high-dollar drugs – on a preferred drug formulary, it will often give a rebate to a PBM, meaning that the PBM will need to negotiate a payment for a drug that is lower than the list price.
From there, the PBM receives reimbursements from its payer partners, while paying a drug dispensing and an administrative fee to pharmacies.
But this rebates and price negotiation process can be flawed, some stakeholders say.
For one, this process is left mostly opaque. It's hard to know rebate values, the Commonwealth Fund reported in a separate March 2019 study. Information about drug rebate amounts is kept private in manufacturer and PBM contracts, so it is difficult for payers, consumers, and other stakeholders to know how much anyone may benefit from a rebate.
Furthermore, the process might incentivize PBMs to put higher-cost drugs on formulary lists, resulting in higher spending for the payer and potentially the patient.
“Because they often receive rebates that are calculated as a percentage of the manufacturer’s list price, PBMs receive a larger rebate for expensive drugs than they do for ones that may provide better value at lower cost,” the Commonwealth Fund explained. “As a result, people who have a high-deductible plan or have copays based on a drug’s list price may incur higher out-of-pocket costs.”
Critics have also raised questions about how PBMs pass savings along to stakeholders, including payers, patients, and pharmacies.
PBMs might engage in a practice known as price spreading, for example. As noted above, the PBM receives a drug dispensing and administrative fee from a healthcare payer. The PBM must also pay its own drug dispensing and an administrative fee to pharmacies.
But in some cases, those fees are not equal. When the PBM negotiates a more substantial fee from the payer than the PBM pays to the pharmacy, that constitutes price spreading, and it can be highly lucrative for PBMs.
As the healthcare industry continues to zero in on the rising cost of healthcare and prescription drugs, the role of the PBM and how it works with both payers and drug manufacturers will remain important. These middlemen play a key role in the setting of prescription drug prices, and as such, have a significant effect on healthcare spending, out-of-pocket patient costs, and, ultimately, drug affordability and access.
